Type 2 Diabetes and RA Linked at the Core?
Insulin resistance is independently associated with body mass index (BMI) and synovitis in rheumatoid arthritis patients, shows new research published in Arthritis and Rheumatology.
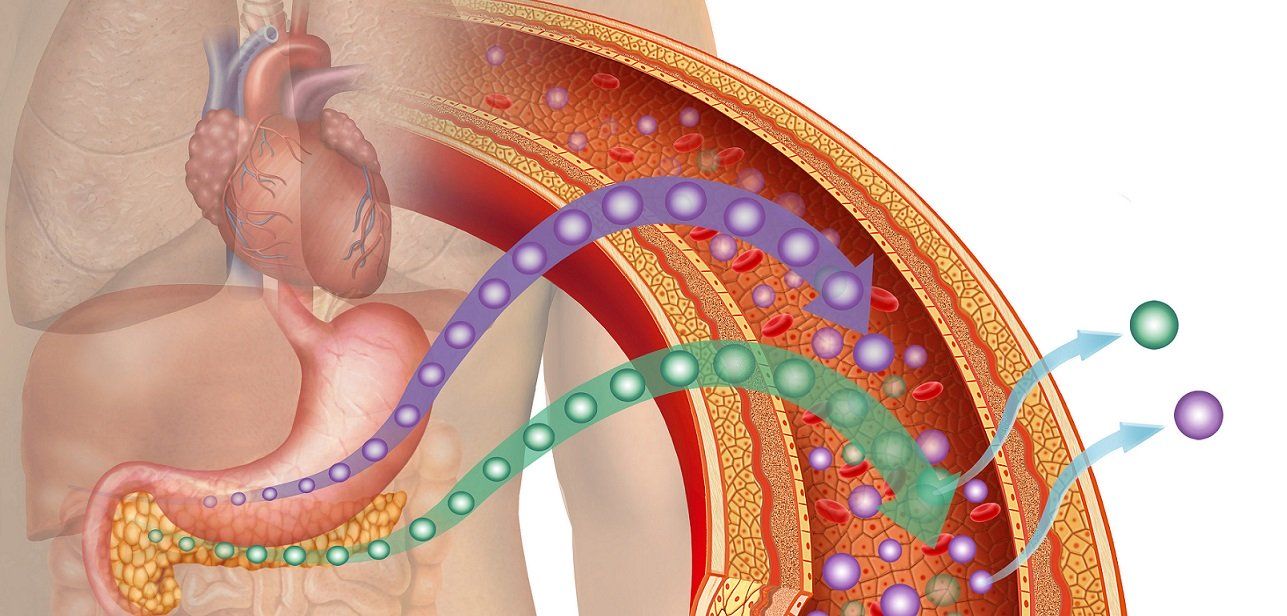
Insulin resistance can increase glucose leading to diabetes and heart disease, but it may also have a role in rheumatoid arthritis flares, shows a new study. (©IlusMedical,AdobeStock_250884023)
Insulin resistance is independently associated with body mass index (BMI) and synovitis in rheumatoid arthritis patients, shows new research published in Arthritis and Rheumatology.
Led by Ronan H. Mullan of the Trinity Centre for Health Science in Dublin, Ireland, researchers wrote that the findings, which were published December 16, suggest a link between glucose levels and rheumatoid arthritis (RA) inflammation.
RA and type 2 diabetes mellitus (T2MD) share many of the same characteristics. Both are powered by abnormal glucose metabolism and both are associated with insulin resistance and adverse cardiovascular disease outcomes.
In this study, researchers recruited 92 rheumatoid arthritis patients (mean age 59, 66% female) who were assessed for insulin resistance, BMI and rheumatoid arthritis disease activity. Researchers found that glucose transporters GLUT1 and GLUT4 were heightened in the synovial tissues of rheumatoid arthritis patients, but not in those of osteoarthritis patients. And, GLUT1 was present in increased levels within all layers of the RA synovium. This suggests an independent association between insulin resistance (particularly with obesity) and the degree of RA disease activity and synovitis.
RELATED: Diabetes and RA: Explaining the Similarities
“This data provides direct evidence that insulin resistant pathways are preferentially expressed within inflamed tissues in RA. And, they suggest a potential mechanism by which the reprogramming of glucose handling through differential GLUT expression favors the perpetuation of inflammation,” researchers wrote.
METFORMIN
Taking metformin, a first-line treatment for type 2 diabetes mellitus, was shown to reduce inflammation in synovial tissue of at least five patients by decreasing the spontaneous production of IL-6, IL-8 and MCP-1 in synovial cells and fibroblasts.
“We confirmed that metformin treatment increased the phosphorylation of AMPK and reduced the expression of GLUT1 from synovial fibroblasts. Furthermore, we demonstrated that metformin is capable of altering the cellular metabolic activity. This is consistent with recent studies suggesting metformin promotes resolution of inflammation through altered cellular metabolic activity,” researchers wrote.
THE FINDINGS
- Insulin-resistance was independently associated (95% CI) with BMI (p<0.001,n=61) and SJC28 (p=0.008, n=61).
- Glucose transporter GLUT1 expression was greater in the synovium of RA patients as compared to osteoarthritis patients (p=0.0003, n=26 & 16).
- GLUT1 was found to be more evidence in the synovium lining, sub-lining and vascular regions.
- However, GLUT4 expression was decreased in RA as compared to osteoarthritis synovium lining (p=0.0358, n=21 & 8).
- GLUT1 protein expression was decreased in parallel with increased P-AMPK protein expression in primary synovial fibroblasts in four patients treated with metformin.
- Metformin increased glycolytic activity (p<0.05), and decreased OxPhos (p<0.05) in seven RA synovial fibroblasts.
- Metformin or the presence of AICAR decreased spontaneous production of IL-6, IL-8 and MCP-1 in RA synovial cells and synovial fibroblasts.
REFERENCE: Lorna Gallagher Sian Cregan Monika Biniecka, et al. "Insulin Resistant Pathways are associated with Disease Activity in Rheumatoid Arthritis and are Subject to Disease Modification through Metabolic Reprogramming; A Potential Novel Therapeutic Approach," Arthritis and Rheumatolology. Dec. 16, 2019. https://doi.org/10.1002/art.41190